The majority of people know, even above, what is the paper that platelets have in the body: they are blood cells that mobilize when an injury occurs in the blood vessels, forming a platelet cap that helps stop bleeding. This process, known as coagulation, is vital to maintain the integrity of the circulatory system and avoid internal bleeding.1
Beyond this notion, the knowledge he had of these small cells until a few days ago was not much deeper. Neither the number we had to have in blood, nor how they produced or their life . As a child he had been familiar with them because my brother was diagnosed with von Willebrand's disease, a disorder of genetic origin that affects coagulation and that is characterized by having very low levels of von Willebrand factor - a protein that circulates through the blood and that it is also present in blood vessels, so that, when bleeding is produced, this factor is exposed and allows platelets to adhere to start coagulation. Without this factor, coagulation is barely produced. This disease owes its name to the hematologist Eric von Willebrand, who in 1924 described the case of a family of the Åland islands that had coagulation problems. 2,3 Although I touched me closely, platelet biology was a mystery to me. Maybe one does not begin to internalize things until they really touch oneself.
Last Monday, May 6 (2024) I woke up with blood stains on my tongue and lips. I had been with fever and gastroenteritis for several days, so I thought it was perhaps getting worse and decided to go to emergency. Seeing small bleeding in visible parts of your body only put the imagination in operation, which leads to asking you what will happen in those places that you cannot see. From the Emergency of the Primary Care Center they derived directly to the Emergency Department of the Sant Pau Hospital in Barcelona. In addition to the most visible bleeding, it had multiple dots of the head of the head of a pin by legs, abdomen and neck, which are known as petechiae. They asked for different tests, including blood analysis, and while I was waiting lying on a stretcher making plans in my head for that same afternoon, the doctor who had attended me came and told me that my platelet count was 1,000 per microliter. For his expression and for the phrase that came later I sensed that they were very few. “Today, tomorrow, last, and we will see if the following days, you will have to pass them admitted to hematology. If the minimum threshold is 150,000 platelets per microlitro, now you have a 1,000 ”count.
How could my body stay with so few platelets? Was it a problem that my bone marrow could not produce them or there was another cause? At that time, by discarding and after assessing all the tests they had done to me, the diagnosis they gave me was idiopathic thrombocytopenic purple (commonly known as immune thrombocytopenia or PTI ). The infection that had had me in bed the previous week had presumably produced an autoimmune reaction that had caused my immune system to end most of my body's platelets.
My body was able to generate new platelets, but my immune system, without apparent cause, eliminated them. First of all, how are platelets generated? These cells occur mainly in the bone marrow from the differentiation of hematopoietic stem cells in megacariocytes . These cells are very special, since, instead of having a single simple nucleus, they have a large lobed nucleus with multiple copies of the genetic material. This causes megacariocytes to be exceptionally large cells, with a diameter of 50 to 100 μm, compared, for example, with monocytes - the progenitor cells of macrophages - that measure around 12 to 20 μm. When the moment of maturation has come, in a kind of controlled explosion, they can lead to more than a thousand platelets that end up traveling through the blood, ensuring stability in blood circulation (Figure 1). 1 In addition, it has been described that this platelet production does not only happen in the marrow. A study published in Nature revealed that megakaiocytes travel from the bone marrow to the lungs, being able to represent approximately 50% of the total platelet biogenesis, which is equivalent to around 10 million platelets per hour. 4
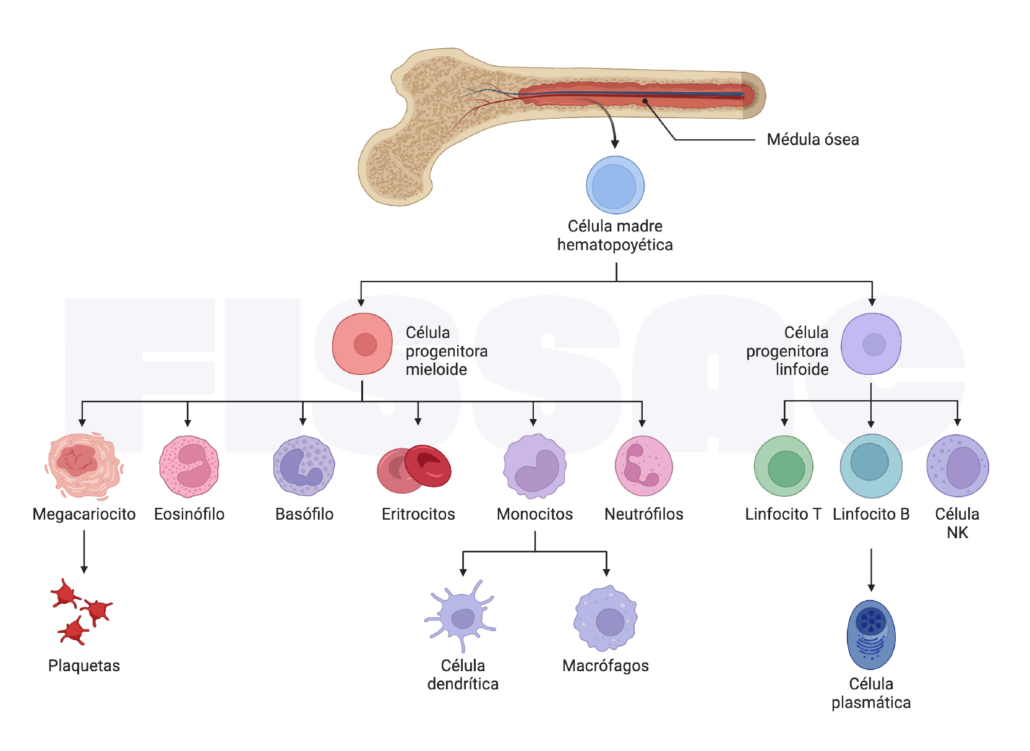
Figure 1. Differentiation of stem cells in the bone marrow. Process in which multipotent stem cells of the bone marrow differ in specific cell types such as red, white and platelets, essential to maintain the blood population of the body.
In a normal course in the life of platelets, these can circulate in the blood for 7-10 days and then eliminated in the spleen or liver. 1 How can the immune system eliminate without any apparent cause cells that are fundamental to life? The body is a miracle of nature that works almost as a perfect machine. However, on very rare occasions you can fail. This makes the incidence of an autoimmune disease such as the PTI among the population very low, of only 2-4 cases per 100,000 people a year. Although some patients have an episode of PTI followed by immediate remission, the PTI develops chronicly in up to 70% of adults with this condition. 5
Our immune system is highly regulated to protect us from bacteria, viruses and premalignant cells in order to preserve health and prevent diseases such as cancer. On very rare occasions it fails. The first time that the immune system could be recorded by the platelets was in a very bold experiment carried out by the hematologist Dr. William Harrington in 1951 . 6 Intrigued by the cases of patients suffering from severe bleeding without a clear cause, Harrington infused a patient with PTI , predicting that if the plasma contained some factor that affects platelets, he himself would experience similar symptoms. Indeed, shortly after the infusion, their number of platelets decreased dramatically, suggesting that the immune system of patients with PTI was producing autoantibodies that erroneously eliminated their own platelets.
Why can the immune system destroy platelets?
While the causes are not yet clear, some of the mechanisms involved in the destruction of platelets by the immune system are currently known. One of these mechanisms involves autoantibodies produced by B cells, a type of lymphocyte specialized in the generation of antibodies that normally fight viruses and bacteria. In the case of the PTI, these autoantibodies are wrongly directed against platelets . This self -reactive behavior of B cells can be triggered by viral infections that alter immune regulation (such as the one I could have), or by a genetic predisposition that interferes with immune tolerance.
Once the autoantibodies bind to platelets, they mark them for destruction. This marking facilitates the recognition of platelets by macrophages in the spleen and liver, which phagocythe and destroy them . Therefore, in some cases in which the first proposed treatments do not work, the removal of the spleen (splenectomy) is proposed, since in addition to being an organ in which the platelets are eliminated, it also plays a role in the production of autoantibodies They attack platelets. 5.7
On the other hand, autoantibodies also affect the biogenesis of platelets attacking megakaiocytes , interfering in their ability to produce new cells by decreasing the total number of platelets in the circulation. The fragments of the destroyed platelets are exposed by antigen presenting cells through the major class II histocompatibility complex to T lymphocytes, which can stimulate additional immune responses against platelets and perpetuate the autoimmunity cycle. This type of lymphocytes, which in a context for example of cancer are dedicated to attacking tumor cells, in a PTI eliminate platelets. 8 The continuous activation of these T cells can lead to an imbalance in T subtypes, promoting an increase in pro -inflammatory cells such as TH1 and TH17, and a reduction in regulatory T cells, which are responsible for suppressing the inflammatory function To avoid autoimmune attacks, exacerbating the destruction of platelets. A perfect storm is created that destroys platelets without an apparent cause (Figure 2).
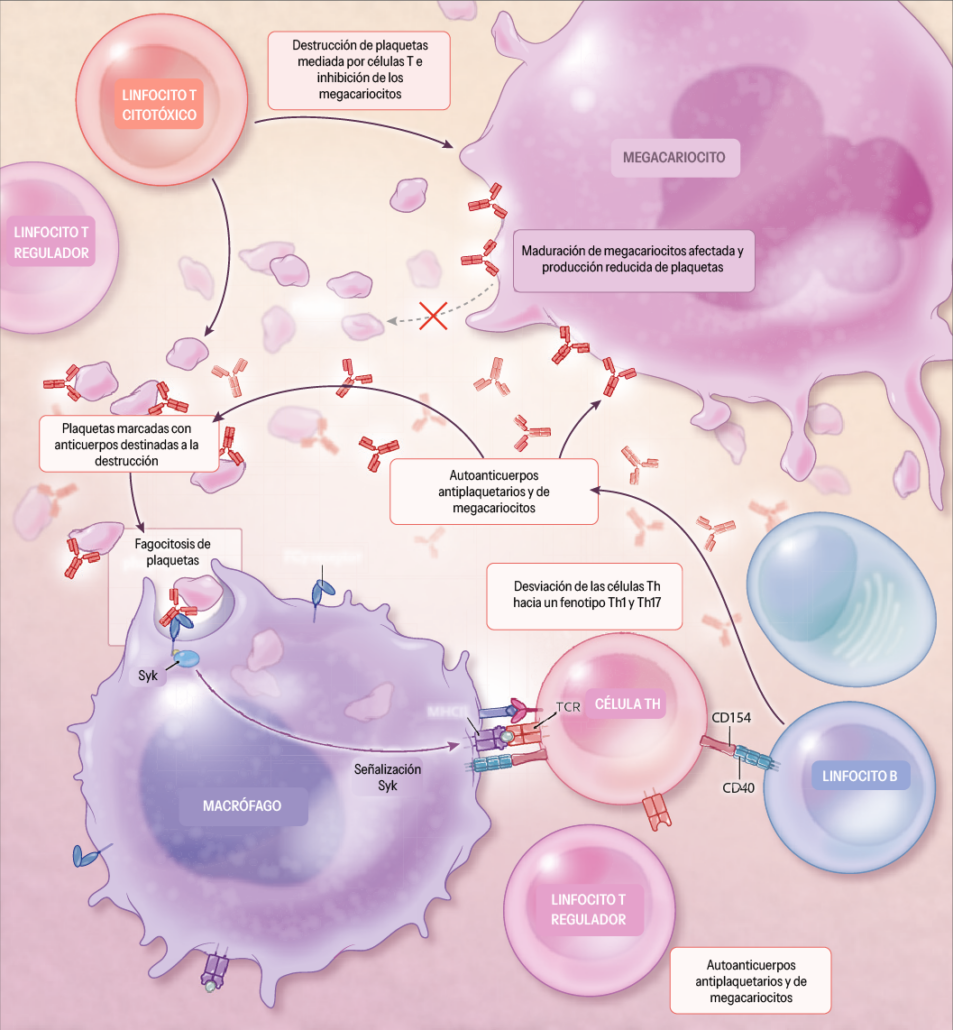
Figure 2. mechanisms involved in immune thrombocytopenia . Adapted from Cooper et al. New England Journal of Medicine, 2019. 5
Because the immune system is runaway, glucocorticoid treatment is standard initial therapy for patients with PTI mainly due to its powerful anti -inflammatory and immunosuppressive effect. Although between 60 and 80% of these patients show an initial response to glucocorticoids, only between 30 and 50% of adults have a sustained response after glucocorticoids are suspended.5,9
In my case the treatment worked in this first phase. I entered Monday with 1,000 platelets per blood microliter, Tuesday's count was 2,000, Wednesday 20,000, and Thursday 40,000. Even though well below the minimum threshold, glucocorticoids were getting blood platelets. Although we still do not know if I will be part of that 70% of people whose PTI episode becomes chronic, the risk of internal bleeding was decreasing.
God does not play the dice, or yes?
Many times we hear that life changes in a second. You go to the doctor thinking that it will give you a treatment for a simple flu and you end up sleeping at the hospital sharing a plant with patients with diseases such as leukemia. My episode has only been a call for attention and is not comparable to what those people who really do not know if they will be able to survive the disease. However, each in his situation is asked many questions almost always without response: why me? Why in a matter of hours my blood has run out of platelets turning my body into a watchmaking pump? Will it happen to me again ?
My roommate, training doctor, with a serious illness ahead, always with good gesture and how are you today Adrián? He told me in one of our first conversations that in life (and in disease) chance It is an unpredictable element that can change reality for no apparent reason. Not everything that happens to us has a cause. Albert Einstein, father of modern physics, was reluctant to accept the principle of uncertainty and chance in the quantum world, preferred to think that " God does not play the dice with the universe ." However, history has shown that chance plays a much more decisive role than we would like to admit. In our world, many chronic diseases that afflict us today, such as cardiovascular or some types of cancer, are related to our current lifestyle and exposure to polluting agents. Others are simply due to random.
In those moments of uncertainty, the only certainty that made me feel safe and protected was the health system itself, public health. The Oncohematology plant in which many people fight diseases in balance with life became a space of tranquility. It may sound like Mantra, but health in Spain is a privilege that we are not aware of. And look at everyone equally. In that maelstrom of people and stress everything works perfectly. And always with good faces. When you see your life to pass, the protection of doctors, nurses, wardens and cleaning personnel is so effective that even at those moments you do not know what will happen, you feel safe. Public health is the central element on which a country that takes care of its citizens must pivot. And you have to defend it.
What can happen to you in a country like the United States without a state of public and universal well -being? a world that appears more and more to individualism, in which social inequalities seem Be able to continue living.
References:
1. Van der Meijden Pej, Heemskerk Jwm. Palelet Biology and Functions: New Concepts and Clinical Perspectives. Nat Rev cardiol . 2019; 16 (3): 166-179. DOI: 10.1038/S41569-018-0110-0
2. Mukherjee S. The Song of the Cell: An Exploration of Medicine and the New Human . Simon and Schuster; 2022.
3. Nilsson im. The History of von Wilbrand Disease. Haemophilia . 1999; 5 (S2): 7-11. DOI: https: //doi.org/10.1046/J.1365-2516.1999.0050S2007.x
4. Lefrançais E, Ortiz-Muñoz G, Caudrillier A, et al. The lung is a site of plalet bio -biogeir for hamatopoietic progenitor. Nature 2017; 544 (7648): 105-109. DOI: 10.1038/Nature21706
5. Nichola C, Waleed G. Immune Thrombocytopenia. New England Journal of Medicine . 2019; 381 (10): 945-955. DOI: 10.1056/NEJMCP1810479
6. Harrington WJ, Minnich V, Hollingsworth JW, Moore C V. Demonstration of a Thrombocytopenic Factor in the Blood of Patients with ThrombomcoCyTopenic Purpura. J LAB CLIN MED . 1951; 38 (1): 1-10.
7. Kojouri K, Vesely Sk, Terrell Dr, George Jn. Splenectomy for adult patients with idiopathic thrombocytopenic purple: a Systematic Review to Assess Long-Term Palelet Count Responsible, Prediction of Response, and Surgical Complications. Blood 2004; 104 (9): 2623-2634.
8. Olsson B, Andersson Po, Jernås M, et al. T-Cell-Mediated Cytotoxicity Toward Palelets in Chronic Idiopathic Thromtopepenic Purple. Nat med . 2003; 9 (9): 1123-1124. DOI: 10.1038/NM921
9. Frederiksen H, Ghanima W. Response of First Line Treatment With Corticosteroids in A Population-Based Cohort of Adults With Primary Immune Thrombocytopenia. EUR J INTER . 2017; 37: E23-E25. DOI: 10.1016/J.EJIM.2016.09.001
A comment
I await your prompt recovery. That in this emotional situation you have written this article says a lot about a person, which puts knowledge and their experience for others to learn. The conclusion of the article under the title "God does not play the dice or if" is one of the best lines I have read in time for his ability to make you reflect. Thank you for sharing knowledge and experience.
A big hug and encouragement